MOLECULE
- sc-uPA in keratinocyte-melanocyte interaction inhibition
- Promotion of Autophagy, alteration of dermal structures, and decrease in Mast cells
- PAR-2 and LL-37 inhibition
Regimen Lab Skincare Encyclopedia
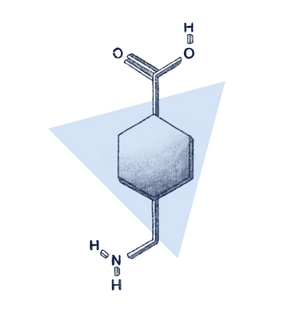
Tranexamic Acid
V 1.0
Regimen's Take
Tranexamic acid (TXA) is a great skincare active for dealing with hyperpigmentation and barrier repair. It’s an up and coming ingredient that shows a lot of promise for treating UV-induced pigmentation and melasma. Use it at 3-5% (greater than 5% doesn’t show added benefits and would just cause irritation), and make sure that the solution is formulated for enhanced penetration. TXA is relatively stable with pH changes, exposure to light or oxygen, so degradation is not a concern, especially at neutral pH. Although great on its own, TXA shows better results when combined with 5% Niacinamide, 2% Alpha Arbutin, 1% Kojic Acid, Azaleic Acid, Boswellic Acids and other proven actives. Use it topically twice a day, and results are usually seen after 8-12 weeks. Since its penetration is not stellar, you can use it after chemical exfoliation with AHAs or BHA, microneedling, or other techniques such as Intense Pulsed Light (IPL) to get the best results. We need to see more high-quality RCTs properly controlled for vehicle and sunscreen use, tested against the Kligman Formula or the Triple Combination Cream.
TLDR
- It is an excellent adjunct therapy for hyperpigmentation
- Depending on the formulation, it can penetrate the border between the epidermis and dermis where it exerts its effect
- Its primary mechanism of action is preventing the activation of Plasmin that leads to pigmentation
- It can also help promote the barrier by upregulating Tight Junctions (TJ) in between cells
- It is a good candidate active for Rosacea as it restores lamellar lipid secretion
What is Tranexamic Acid?
Tranexamic acid is a chemically-synthesized amino acid lysine analog used to treat heavy bleeding during surgery. It was first characterized in 1979 by Nijo Sadako while treating a patient with chronic urticaria (itchiness) who had melasma. Sadako made an accidental discovery that oral administration of Tranexamic acid (TXA) significantly reduced the intensity of melasma within a period of two to three weeks.[1]
What is Melasma?
Melasma, (aka chloasma), is a common acquired condition of pigmentary disorder marked by irregular hyperpigmented macules or patches common in females with dark skin types living in areas with intense ultraviolet (UV) light exposure.[2] It is usually caused by the following:[3]

Avoiding the causes of melasma is the best way to guard against it’s appearance. Wearing sufficient, high-quality sunscreen, avoiding harmful ingredients, treating and preventing acne, and inflammation can help prevent many skin pigmentation types.
In terms of treatment, Hydroquinone (HQ) is, unfortunately, still considered as the gold standard of treatment for melasma, albeit its potential to cause irritation. HQ is used at a concentration of 2-4%, usually in combination with other ingredients. These combinations are as follows:[4][5]
 The use of TXA has become more popular over the last few years. (Side note: When we first started researching TXA in 2018, only a couple of journals were published. The works of Maeda et al. were significant in our decision to include it in our formulation.) We’ll explain how it penetrates, how it works, and the different clinical trials showing its efficacy in the following sections.
The use of TXA has become more popular over the last few years. (Side note: When we first started researching TXA in 2018, only a couple of journals were published. The works of Maeda et al. were significant in our decision to include it in our formulation.) We’ll explain how it penetrates, how it works, and the different clinical trials showing its efficacy in the following sections.
Does it Penetrate?
TXA is a hydrophilic (water-loving) molecule that does not preferentially bind to proteins in the skin. It’s ability to penetrate is formulation dependent[6], and requires the use of formulation enhancers. In a vertical Franz diffusion cell study, two formulations of TXA were compared and showed different penetration gradient in the skin. Although dermal penetration is less likely, it can reach a sufficient effective dose in the viable epidermis, where TXA mainly exerts its action. This means that TXA is great for preventing active pigmentation, especially epidermal melanin. Dermal pigmentation, on the other hand, is harder to target as melanophages (a type of phagocytes) ingests melanin in the epidermis and carries it to the lower part of the dermis. Once lodged on the dermis, it could take years before that dermal pigmentation degrade. That’s why so many of us have those pesky spots that won’t go away. TXA has some effect on these types of pigments, but since its penetration in the dermis is limited, it cannot remove dermal spots on its own.
Several adjunct methodologies have also been investigated to improve the efficacy of tranexamic acid. Microneedling, Intense-Pulsed Light (IPL), lasers, and intradermal injection have shown promise to improve TXA penetration.
How does it work?
1) Through Plasmin Inhibition
When the skin is injured through cuts, chemical burns, SLS-based surfactant damage, tape-stripping, or UV exposure,[7] your skin cells produce a compound called Plasminogen Activator (PA),[8] which is responsible for activating Plasminogen into Plasmin. Plasminogen is the precursor for Plasmin (the suffix gen means “the precursor of”), and it exists in human epidermal basal cells.[9] Plasmin, a serine protease, is responsible for initiating wound healing by activating keratinocyte proliferation and migration. It also starts several processes that lead to inflammation, melanogenesis, and other processes as a potent initiator.
Plasmin’s production in the skin is one of the triggers of inflammation because it activates several signaling pathways that lead to the production of cytokines (inflammatory messengers), ROS, and other mediators.[10] Exposure to UV triggers Plasmin to activate phospholipase A2,[7:1][11][12] which participates in arachidonic acid production, one of the most important inflammatory mediators. Arachidonic acid is then processed to various compounds such as Prostaglandin E2 (PGE2)[13] and Leukotrienes (LT)[14]. PGE2 and LT are the compounds responsible for causing fever when you have an infection or inflammation. Aside from their inflammatory role, they also are potent melanogenic factors that tell your melanocytes to overproduce melanin.[15][16] Plasmin also enhances the release of an alpha-melanocyte-stimulating hormone (α‑MSH), which tells your melanocytes to activate and produce more melanin. Plasmin is also reported to participate in cytokine expression and activation, production of active peptides, and phosphorylation of transcription factors.[17][18][19][20]
To find out more about how TXA works on pigmentation, we need to discuss a few cell structures and the molecules they produce. Human keratinocytes contain two types of Plasminogen Activators (PA): urokinase-type PA (uPA) and tissue-type PA (tPA),[8:1] but they only secrete the one type of uPA, which is the single-chain uPA (sc-uPA).[21] uPA plays a role in keratinocyte growth and differentiation[22] and migration through an autocrine fashion.[23] Human Melanocytes, on the other hand, primarily produce tPA, rarely uPA.[24]
Tranexamic acid is structurally similar to the amino acid lysine. Since both uPA and tPA have receptor binding sites that are lysine-binding, TXA binds readily to these sites, resulting in a conformation change. As a result, TXA suppresses sc-uPA binding to cell membrane receptors, thereby preventing Plasminogen’s activation to Plasmin. TXA’s anti-plasmin activity makes it a great candidate for inhibiting melanogenesis by inhibiting keratinocyte-melanocyte interaction through the inhibition of the plasminogen-plasmin system. To prove this, Maeda et al. used Keratinocyte Conditioned Medium (similar to Keratinocyte extract) to induce tyrosinase activity in melanocytes. They found that KCM from the growth phase induced Tyrosinase more strongly than the confluent phase in human melanocyte cultures. This shows that the growth of keratinocytes plays an essential role in melanin synthesis. They then tested whether TXA can inhibit Tyrosinase induction by KCM, and results showed that TXA is a potent inhibitor of Tyrosinase by inhibiting sc-uPA from activating Plasmin. This inhibition results in a less free Arachidonic Acid (AA), diminished ability to produce PGs, and reduced melanogenesis in melanocytes. This provided further proof of the previously-discussed lysine binding theory.[25] A previous investigation revealed that Topical TXA has a dose-dependent preventative effect on post-UV induced pigmentation from seven days onwards but had no effect on non-exposed skin.[26] In pregnant women and in those using oral contraceptives, serum PA level is also increased.[27] This correlates to the increase in pigmentation that is seen during pregnancy and oral contraceptive use. PA in the skin might participate in hyperpigmentation, and TXA might act through this mechanism.
2. Through Regulation of Autophagy
Another way TXA regulates melanogenesis is through the regulation of Autophagy (literally “self-eating”), cleaning damaged cells. Autophagy is one of the processes that dictate your skin colour. Light skinned people have a higher Autophagy activity compared to people with darker skin colour.[28] This means that the melanin produced in lighter skin degrades faster because of more autophagosomes in the skin.
(Insert Tyrosinase to melanin flowchart here)
We have mentioned above that Plasmin is a really potent messenger that stimulates various processes by phosphorylating cytokines and other signals. One of these molecules that Plasmin phosphorylates (activates) is Mitogen-Activated Protein Kinase (MAPK). MAPK is one of the activators of Mechanistic Target of Rapamycin (mTOR). Together with Akt, MAPK upregulates mTOR, which leads to the suppression of Autophagy. On the other hand, downregulation is executed by AMPK and the p53 signaling pathway, which promotes Autophagy.[29][30] As a recap, Plasmin activates MAPK, MAPK upregulates mTOR, which suppresses Autophagy leading to decreased melanin degradation.
If Autophagy is upregulated, melanin will be degraded. One of the molecules that play a crucial role in upregulating Autophagy is ERK 1/2.[31][32] Phosphorylated ERK (PERK) interacts with various molecules related to Autophagy such as Beclin-1,[33] Autophagic Modulators WIPI1 (a mammalian homolog of ATG18)[34] and microtubule associated protein light chain 3 (LC3), which are potent regulators for the melanogenesis[35] that regulate the formation of autophagosomes that degrade and eat up melanin.[36] Upregulating ERK also phosphorylates MITF, which leads to its degradation. MITF promotes Tyrosinase and TYR 1/2, which are the main enzymes responsible for melanin production.
As we’ve discussed in previous articles on melanogenesis, Tyrosinase is involved in converting Tyrosine to L-dopaquinone, while TRP-2 functions as a DOPA chrome tautomerase that catalyzes the rearrangement of DOPA chrome to DHICA. TRP-1 subsequently oxidizes DHICA to its carboxylated form leading to the production of eumelanin. Tyrosinase and TRP1/2 are transcriptionally regulated by Micropthalmia-associated transcription factor (MITF) in Melanocytes, which is phosphorylated by extracellular signal-regulated kinase (ERK) 2 resulting in the degradation of MITF via the proteasome-mediated proteolytic pathway.[37]
The study done by Cho et al. 2017 revealed several interesting findings:
Expression levels of phospho-p38, phospho-ERK1/2, Beclin-1, Atg12, and LC3 were increased byTXA by approximately 46%, 17%, 48%, 126%, and 49% respectively. TXA downregulated the expression of p-mTOR by approximately 65%, suggesting that TXA can induce the upregulation of autophagy-related proteins, including Beclin-1, Atg12, and LC3, by activating the ERK 1/2 signaling pathway
Autophagosomes (evidenced by LC3 staining) appeared more clearly in the cells treated with the same concentrations of TXA and TGF-B as a positive control in the presence of a-MSH. Results suggest that TXA can lead to the formation of autophagosomes.
Phosphorylation of ERK1/2 results in the degradation of MITF, which in turn downregulates the expression of melanogenesis-associated proteins such as Tyrosinase and TRP1/2, leading to the suppression of melanogenesis. ERK1/2 and p-ERK1/2 were increased to 18% and 5%, respectively. In contrast, the levels of MITF, Tyrosinase, and TRP 1 were significantly decreased to 17%, 14%, and 5%, respectively, compared to that of non-treated control when the cells were treated with 1 mg/ml of TXA for 24 h in the presence of a-MSH. These results suggest that TXA has a synergic action mechanism to exert its anti-melanogenic effect: (1) it can activate the ERK signaling pathway, which leads to the degradation of MITF, which, in turn, downregulates the expression of melanogenesis-associated proteins, including Tyrosinase and TRP1/2; (2) it can also directly suppress the production of the same proteins and enzymes, including MITF, Tyrosinase, and TRP 1/2.
The treatments decreased the melanin production rates with TXA in dose-dependent manners; in particular, the treatment of 4 mg/ml of TXA resulted in decreased melanin synthesis to approximately 46% compared to that observed in cells treated with a-MSH only. The skin whitening effect by TXA through its suppressive ability to the melanin synthesis could also be observed in a melanoderm 3D skin tissue model. After 12 days, TXA’s whitening efficacy was estimated to be approximately twice stronger than arbutin, known to have a good whitening effect. All these results strongly suggest that TXA can inhibit the melanin synthesis in melanoma cell lines and skin tissue.
The reverse-genetics approach using siRNAs targeting mTOR and Atg5 mRNAs showed the inhibitory effect of TXA on the melanin synthesis. This inhibitory effect was relieved significantly in the cells transfected with the siRNAs specific to mTOR and Atg5 for 52 h.
All of these findings show the process by which TXA affects authophagy which leads to the decrease of melanin content in vitro.
TXA was also studied on whether it acts on Tyrosinase using B16 melanoma cells. TXA was able to decrease melanin content by inhibiting the catalytic reaction of Tyrosinase with tyrosin. Since TXA is structurally similar to Tyrosine, it acts as a competitive inhibitor for tyrosinase activity.[38] However, another study done on pure melanocyte cultures showed that it did not inhibit melanin synthesis.[25:1] In 2007, Seong et al. incubated neonatal foreskin cultured melanocytes with TXA. They showed a significant decrease in the number of melanocytes, decreased tyrosinase activity, tyrosinase-related protein TRP1/2, and melanin content in 48 h with increased TA concentration in the culture medium after UVB irradiation. However, there was no change in the number and length of melanocyte dendrites.[39] All of this points to the conclusion that the main mechanism of TXA in pigmentation is through inhibition of the interaction between keratinocytes and melanocytes through inhibition of sc-uPA.
3. Through Changing the Dermal Structures
When your skin gets injured or exposed to UV, your cells move to the injury site to repair the damaged skin structures. They move to those sites through the capillaries or blood vessels in your skin. If your skin continually experiences UV damage, it will thicken and form new capillaries (Angiogenesis) and other new blood vessels (Neovascularization) so that repair cells can easily access the site. This leads to the appearance of solar elastosis in your skin, which looks yellowish and appears thick and wrinkly. Aside from the UV-induced production of melanin, Plasmin also participates in the release of Basic Fibroblast Growth Factor (BFGF) and Vascular Endothelial Growth Factor (VEGF).[40] BFGF, together with VEGF, are potent melanocyte growth factors and potent Growth Factors involved in Angiogenesis (production of new capillaries)[41] and Neovascularization (production of new vascular structures). Aside from that, VEGF interacts with VEGF receptors present in epidermal keratinocytes, releasing metabolites of AA and Plasminogen from the proliferated vessels, further enhancing melanogenesis.[42][43][44]
By inhibiting Plasmin, TXA lowers BFGF and VEGF levels to minimize the skin’s abnormal restructuring, leading to yellowing, wrinkle formation, and hyperpigmentation. These mechanisms point out that TXA may be indicated for other conditions like periorbital melanosis and even early keloids, where the vascularity component can be targeted.[45][46] However, other researchers showed that although TXA decreased the CD31+ blood vessels in the skin, the change was minimal and was not statistically significant. VEGF expression was also downregulated but again not statistically significant. They concluded that TXA has limited capacity to modify dermal structures due to its limited dermal penetration. An alternative mechanism that they proposed is through Endothelin (ET) suppression. ET-1 is thought to be secreted from keratinocytes, and it is a well-known melanogenic factor that induced pigmentation and the tanning response upon UV irradiation.[47][48] Although TXA inhibits Plasmin and Plasmin activates ET-1, more studies are needed to confirm TXA’s role in ET-1 suppression.
4. Through Decreasing Mast Cells
TXA is also able to decrease the number of mast cells in your skin. Mast cells (MC) are like sentinels in your body that target foreign bodies by throwing granule “bombs” to them. These bombs contain various that kill the foreign body and, at the same time, trigger the signal for back-up. These substances include histamine, heparin, and Tryptase. Histamine is the substance that increases your blood vessels’ permeability, so other immune cells can quickly migrate into the action site. Tryptase, on the other hand, is released to destroy bacteria that the mast cells encounter. Repetitive UV exposure also increases the number of MCs and their Tryptase release.[49] Unfortunately, Tryptase also degrades Type IV collagen in the basement membrane of your skin.[43:1] This degradation is one of the many reasons why UV exposure can lead to a weak basement membrane characterized by rough and wrinkly skin. Mast cells also induce vascular proliferation by secreting various angiogenic factors, such as the VEGF mentioned above.[50] Besides, Elastin content (another ECM component) is correlated with the number of mast cells in the skin,[51] and that mast-cell deficient mice do not develop solar elastosis upon UV exposure.[52] These findings support the histologic findings that TXA improves the extracellular matrix (ECM), leading to smoother skin.[53]
How does TXA repair the barrier?
Plasmin is a serine protease that breaks down proteins in the epidermis. It can also activate other proteases in the skin leading to a damaged barrier. In normal levels, proteases help your skin remove dead skin cells on the skin’s upper layers through desquamation. They are also responsible for the hydrolysis of Filaggrin (moisture bombs) in your epidermis to keep your skin hydrated. However, the skin sometimes overreacts and produces high amounts of proteases when injured, leading to epidermal hyperplasia and disrupting the barrier homeostasis. One key example of this is the effect of sun exposure. UVB reduces the Stratum Corneum’s water retention and changes keratin composition and the structure of intercellular lipids.[54]
The effect of protease inhibitors on barrier homeostasis has also been studied. Denda et al. discovered that TA could accelerate skin barrier recovery and inhibit the epidermal hyperplasia induced by repeated barrier disruption in humans.[55] Many researchers have found that tight junctions (TJ) and TJ proteins are involved in barrier formation, serving as a rescue system when the stratum corneum is impaired or missing.[56] Occludin, one of the critical TJ proteins, plays a crucial role in the skin barrier function.[57][58] Katsuta et al. reported that TA could inhibit the physical interaction between urokinase-type plasminogen activator and stratum corneum, which is the reason for the accelerating recovery of barrier function.[59]
Further studies have shown that 5% TXA effectively accelerates barrier recovery and decreases melanin index in UV-irradiated skin. The results show that 5% TXA in specific, was able to accelerate barrier recovery in mice and human skin. This is owed to TX-A’s Plasmin inhibition through the inactivation of urokinase Plasminogen Activator (uPA). Upon 14 days of topical TXA application, there was a significant increase in Occludin compared to the non-treated areas. Occludin is a type of TJ that holds skin cells together, forming the moisture barrier. TXA’s ability to upregulate Occludin shows its ability to accelerate barrier repair. Still, it is advisable to perform more research on Occludin’s upregulation in molecular mechanisms in the future.[60]
Inactivation of PAR-2 and LL-37
Proteases such as Plasmin also activate Protease-activated receptor two (PAR-2), which signals an influx of Ca2 in the stratum granulosum. PAR-2 is a G-protein coupled 7-transmembrane domain receptor, which mediates inflammation in various tissues upon activation by serine proteases (SPs) such as Kallikrein.[61][62] SPs degrade the epidermal anti-microbial peptide to its active form, cathelicidin LL-37, which mediates vascular action and inflammation, Rosacea’s inflammatory characteristics.[63][64][65] Disruption of barrier stimulates cytokine expression, LL-37 expression, and expression of vascular growth factor.[66] This influx of Ca2 inhibits the release of lamellar body secretion, which leads to an impairment of barrier repair.[67]
Lamellar body secretion is your skin’s way to replenish and repair the lamellar bodies that contain Ceramides, Cholesterol, and Fatty Acids in your SC. PAR2 activation also decreases E-cadherin, which is also essential in epidermal barrier repair.[68][69][70] Increased Proteases in your skin also degrade the anti-microbial peptide cathelicidin LL-37 to its active form. LL-37 mediates vascular action and inflammation, which are the features of Rosacea. TXA accelerates barrier recovery through SP inhibition and inhibits epidermal hyperplasia induced by repeated barrier disruption.[60:1] TXA was shown to inhibit proteases that activate PAR-2 signaling and LL37 activation.[71] Further studies proved its efficacy as a cheap treatment option for improving barrier homeostasis in Rosacea.[72]
Clinical Trials
Actives |
Conclusion |
Source |
5% TXA |
5% TXA reduces TEWL in mice and human skin showing that certain protease inhibitors are capable of accelerating barrier repair. |
Denda, M., Kitamura, K., Elias, P.M., et al. (1997) Trans-4-(Aminomethyl)cyclohexane carboxylic acid (T-AMCHA), an anti-fibrinolytic agent, accelerates barrier recovery and prevents the epidermal hyperplasia induced by epidermal injury in hairless mice and humans. J Invest Dermatol ; 109: 84–90. |
2% TXA emulsion |
n=25, 5-18 weeks. TXA showed improvement in pigmentation |
Konda, S., Okada, Y., & Tomita, Y. (2007). Clinical study of effect of tranexamic acid emulsion on melasma and freckles. Skin Res, 6, 309–15. doi: https://doi.org/10.11340/skinresearch.6.3_309 |
10% TXA daily + weekly iontophoresis vs daily 10% TXA alone |
n=33, 12-week prospective randomized double blind split-face study showed that iontophoresis showed faster results. Topical TXA only showed effects after 7 weeks, only marginal reduction in the area. Note: both groups used sunscreen |
Arora, R., & Sharma, R. (2009). Study on Effectiveness and Safety of Combination of Daily 10% Tranexamic Acid Gel Application and Weekly Iontophoresis Versus Daily 10% Tranexamic Acid Gel Alone in Treatment of Melasma. Galore International Journal Of Health Sciences And Research, 4(1), 99-106. |
3% TXA 2x daily vs weekly TXA injection. |
n=18 12-week open, comparative, randomized trial showed no statistical difference between both groups. |
Steiner, D., & Addor, F. (2009). Study evaluating the efficacy of topical and injected tranexamic acid in treatment of melasma. Surgical And Cosmetic Dermatology, 1(4), 174-177. |
5% TXA |
n=23, 12 weeks. No difference between 5% TXA and Vehicle. NOTE: unscreen use for both groups. |
Kanechorn Na Ayuthaya, P., Niumphradit, N., Manosroi, A., & Nakakes, A. (2012). Topical 5% tranexamic acid for the treatment of melasma in Asians: a double-blind randomized controlled clinical trial. Journal of cosmetic and laser therapy : official publication of the European Society for Laser Dermatology, 14(3), 150–154. https://doi.org/10.3109/14764172.2012.685478 |
5% TXA vs Vehicle |
n=23, 12-week randomized, double-blind, split-face, prospective study showed decrease in MASI on both sides, no statistical difference between TXA and vehicle. Note: Both group used SPF 60 |
Kanechorn Na Ayuthaya, P., Niumphradit, N., Manosroi, A., & Nakakes, A. (2012). Topical 5% tranexamic acid for the treatment of melasma in Asians: A double-blind randomized controlled clinical trial. Journal Of Cosmetic And Laser Therapy, 14(3), 150-154. doi: 10.3109/14764172.2012.685478 |
2% TXA, 2% Niacinamide + Oral TXA |
n=25, 8 weeks. Histologic findings show that there is a reduction of epidermal pigmentation, vessel number and mast cell count. MI and EI through Mexameter were also reduced. |
Na, J., Choi, S., Yang, S., Choi, H., Kang, H., & Park, K. (2012). Effect of tranexamic acid on melasma: a clinical trial with histological evaluation. Journal Of The European Academy Of Dermatology And Venereology, 27(8), 1035-1039. doi: 10.1111/j.1468-3083.2012.04464.x |
2% Niacinamide + 2% TXA vs Vehicle |
n=42, 8-week randomized, double-blind,vehicle-controlled trial showed txa is more effective than vehicle in reducing pigmentation beyond sunscreen. |
Lee, D., Oh, I., Koo, K., Suk, J., Jung, S., & Park, J. et al. (2013). Reduction in facial hyperpigmentation after treatment with a combination of topical niacinamide and tranexamic acid: a randomized, double-blind, vehicle-controlled trial. Skin Research And Technology, 20(2), 208-212. doi: 10.1111/srt.12107 |
Microneedling + 4% TXA vs microinjection +4% TXA |
n=60, 1-year prospective, randomized, open-label study showed significant decrease in MASI scores in both groups. No difference between groups. |
Budamakuntla, L., Loganathan, E., Suresh, D., Shanmugam, S., Dongare, A., & Prabhu, N. et al. (2013). A randomised, open-label, comparative study of tranexamic acid microinjections and tranexamic acid with microneedling in patients with melasma. Journal Of Cutaneous And Aesthetic Surgery, 6(3), 139. doi: 10.4103/0974-2077.118403 |
5% TXA |
5% TXA solution is effective in decreasing the MI value in human damaged skin, which suggests that melanism from UVB irradiation can be rectified by TXA. TXA can significantly accelerate barrier recovery and decrease the melanin index values of ultraviolet B-irritated skin. The mean optic density of Occludin from TXA treatment is higher than from self-repair. This suggests that TXA can accelerate skin barrier recovery and upregulate Occludin induced by physicochemical damages of human skin, but it is advisable to perform more research on the upregulation of Occludin in molecular mechanisms in the future. |
Yuan, C., Wang, X., Yang, L., & Wu, P. (2013). Tranexamic acid accelerates skin barrier recovery and upregulates occludin in damaged skin. International Journal Of Dermatology, 53(8), 959-965. doi: 10.1111/ijd.12099 |
3% Tranexamic acid vs 3% HQ +0.1% Dexamethasone |
n=50, 12 weeks. Significant decreasing trend in both groups; no significant difference in effect but worse side effect in HQ group. Note: Poorly controled study |
Ebrahimi, B., & Naeini, F. (2014). Topical tranexamic acid as a promising treatment for melasma. J Res Med Sci., 19(8), 753-7. |
2% TXA plus IPL vs IPL + vehicle |
n=13, 12 weeks. Randomized split-faced controlled trial showed statistical significant decrease of MI and MASI for TXA + IPL. TXA also prevented rebound pigmentation. |
Jong Yoon Chung M.D., Jong Hee Lee M.D., Ph D. & Joo Heung Lee M.D., Ph D. (2015): Topical Tranexamic Acid as an Adjuvant Treatment in Melasma: Side-by-Side Comparison Clinical Study, Journal of Dermatological Treatment, DOI: 10.3109/09546634.2015.1115812 |
5% liposomal TXA vs 4% HQ |
n=33, 12-week double blind split-faced trial showed that TXA showed greater decrease in MASI score but not statistically different from HQ. More side effects were seen with HQ. |
Banihashemi, M., Zabolinejad, N., Jaafari, M., Salehi, M., & Jabari, A. (2015). Comparison of therapeutic effects of liposomal Tranexamic Acid and conventional Hydroquinone on melasma. Journal Of Cosmetic Dermatology, 14(3), 174-177. doi: 10.1111/jocd.12152 |
Oral TXA |
n=561, 4-year Retrospective analysis showed 89.7% had improvement in melasma |
Lee, H., Thng, T., & Goh, C. (2016). Oral tranexamic acid (TA) in the treatment of melasma: A retrospective analysis. Journal Of The American Academy Of Dermatology, 75(2), 385-392. doi: 10.1016/j.jaad.2016.03.001 |
2% TXA emulsion |
n=23, 12 weeks. Reduction in MASI score, skin biopsies show significant decrease in melanin content, Endothelin-1 (ET-1) was downregulated. |
Kim, S. J., Park, J. Y., Shibata, T., Fujiwara, R., & Kang, H. Y. (2016). Efficacy and possible mechanisms of topical tranexamic acid in melasma. Clinical and experimental dermatology, 41(5), 480–485. https://doi.org/10.1111/ced.12835 |
2.5% TXA |
n=84, 8-week Randomized double-blind trial showed significant difference in MASI scores |
Lu, J., Yang, L., Xu, P., Bian, F., & Zhang, H. (2017). Whitening Efficacy of Tranexamic Acid Cataplasm on Melasma in Chinese Women. Integrative Medicine International, 4(3-4), 154-160. doi: 10.1159/000485101 |
Oral and Intradermal TXA |
n=100, 12 weeks. Both are equally effective in MASI reduction |
Sharma, R., Mahajan, V., Mehta, K., Chauhan, P., Rawat, R., & Shiny, T. (2017). Therapeutic efficacy and safety of oral tranexamic acid and that of tranexamic acid local infiltration with microinjections in patients with melasma: a comparative study. Clinical And Experimental Dermatology, 42(7), 728-734. doi: 10.1111/ced.13164 |
5% TXA vs 2% HQ |
n=60, 12 weeks. Randomized double -blind clinical trial showed that TXA reduced melanin level and MASI score; difference not significant between groups but higher patient satisfaction in TXA than HQ. Note: Both group used SPF 30 |
Atefi, N., Dalvand, B., Ghassemi, M., Mehran, G., & Heydarian, A. (2017). Therapeutic Effects of Topical Tranexamic Acid in Comparison with Hydroquinone in Treatment of Women with Melasma. Dermatology And Therapy, 7(3), 417-424. doi: 10.1007/s13555-017-0195-0 |
Microneedling + 0.5% TXA vs control + 0.5% TXA |
n=28, 12-week trial showed significant increase in effectiveness of TXA using microneedles. TEWL, roughness, skin hydration, skin elasticity, Erythema index showed no significant difference. |
Xu, Y., Ma, R., Juliandri, J., Wang, X., Xu, B., & Wang, D. et al. (2017). Efficacy of functional microarray of microneedles combined with topical tranexamic acid for melasma. Medicine, 96(19), e6897. doi: 10.1097/md.0000000000006897 |
3% TXA, 2% Galactomyces Ferment Filtrate, 4% Niacinamide, 2% Alpha Arbutin vs 4% Hydroquinone |
n=30, 4-week Randomized double-blind clinical trial showed no significant difference between groups. |
Santoso, G., Anwar, A., Tabri, F., Djawad, K., Madjid, A., & Seweng, A. (2018). The Effectiveness of Combination Serum of Tranexamic Acid, Galactomyces Ferment Filtrate, Niacinamide And Alpha Arbutin in Enhancing Skin Brightness. International Journal Of Medical Reviews And Case Reports, 2(Reports in Surgery and Dermatolo), 1. doi: 10.5455/ijmrcr.enhancing-skin-brightness |
10% TXA vs Placebo |
n=40, 12-week split-faced randomized clinical trial showed TXA to significantly reduce MASI score. |
Saka, S., Rao, G., Komaram, R., Kotha, S., Tatavarthi, R., & Chitturi, L. (2018). EFFICACY OF 10% TOPICAL TRANEXAMIC ACID IN MELASMA - A RANDOMIZED PLACEBO-CONTROLLED SPLIT FACE STUDY. International Journal Of Pharmaceutical Sciences And Research, 10(5), 2583-2586. |
3% TXA, 1% Kojic Acid, + 5% Niacinamide |
n=55, 12-week clinical study. Improvement in PIH and pigmentation compared to baseline and control. Note: No randomization. |
Desai, S., Ayres, E., Bak, H., Manco, M., Lynch, S., & Raab, S. et al. (2019). Effect of a Tranexamic Acid, Kojic Acid, and Niacinamide Containing Serum on Facial Dyschromia: A Clinical Evaluation. Journal Of Drugs In Dermatology, 18(5), 454-459. |
5% TXA vs 3% HQ |
n=100, 12 weeks. Both are equally effective in MASI reduction |
Janney, M., Subramaniyan, R., Dabas, R., Lal, S., Das, N., & Godara, S. (2019). A Randomized Controlled Study Comparing the Efficacy of Topical 5% Tranexamic Acid Solution versus 3% Hydroquinone Cream in Melasma. Journal Of Cutaneous And Aesthetic Surgery, 12(1). |
5% TXA vs 2% HQ |
n=354 4-week randomized study showed that mean MASI score was statistically less in HQ group compared to TXA but TXA group developed less side effects. |
Erum, A., Asad, F., Kiran, R., Hussain, I., Hassan, F., & Bashir, B. (2019). Topical tranexamic acid versus hydroquinone for patients presenting with melasma. Journal Of Pakistan Association Of Dermatologists, 29(2), 220-224. |
Microneedling with 5% TXA vs Microneedling with 20% Vitamin C |
n=30, 8-week split face comparative study showed improvement in both, more in TXA but not statistically significant. |
Menon, A., Eram, H., Kamath, P. R., Goel, S., & Babu, A. M. (2019). A Split Face Comparative Study of Safety and Efficacy of Microneedling with Tranexamic Acid versus Microneedling with Vitamin C in the Treatment of Melasma. Indian dermatology online journal, 11(1), 41–45. https://doi.org/10.4103/idoj.IDOJ_22_19 |
Microneedling with 10% TXA vs microneedling |
n=42, 12-week 2 week interval, randomized double blinded-clinical trial. Statistically significant higher decrease in MASI in group 1, Histopathologically, epidermal hyperpigmentation and dermal melanophages were significantly reduced after treatment with more obvious reduction in group I. The number of melanoma antigen recognized by T cells-1-positive cells showed significant reduction in both groups; this reduction was statistically higher in group I than group II. |
Saleh, F., Abdel-Azim, E., Ragaie, M., Guendy, M., (2019), Topical tranexamic acid with microneedling versus microneedling alone in treatment of melasma: clinical, histopathologic, and immunohistochemical study, Journal of the Egyptian Women's Dermatologic Society, 16;2, 89-96 |
Oral TXA + 3% Topical TXA vs Oral TXA + 20% Azaleic Acid |
n=100, 4-month randomized study showed significantly less reduction in oral plus topical TXA compared to oral plus azaleic acid. |
Malik, F., Hanif, M., & Mustafa, G. (2019). Combination of Oral Tranexamic Acid with Topical 3% Tranexamic Acid versus Oral Tranexamic Acid with Topical 20% Azelaic Acid in the Treatment of Melasma. Journal Of The College Of Physicians And Surgeons Pakistan, 29(6), 502-504. doi: 10.29271/jcpsp.2019.06.502 |
Intradermal TXA vs 3% Topical TXA vs TCC ( 2%HQ, 0.025% Tretinoin, 0.01% Flucinolone acetonide) |
n=205, 6-month single-centered, prospective randomized controlled interventional study showed intradermal TXA showed the most statistical reduction follwed by TCC followed by topical TXA. Note: Suncreen use 4X daily. Really impressive results |
Patil, S., & Deshmukh, A. (2019). Comparative study of efficacy of intradermal tranexamic acid versus topical tranexamic acid versus triple combination in melasma. Pigment International, 6(2), 84. doi: 10.4103/pigmentinternational.pigmentinternational_19_1 |
10% TXA + Microneedling vs Microneedling alone |
n=40, 8-week Split-face, prospective, randomized open-label study. Improvement on melasma is more significant with TXA. Notes: Level B; Low Quality |
Kaur, A., Bhalla, M., Pal Thami, G., & Sandhu, J. (2020). Clinical Efficacy of Topical Tranexamic Acid With Microneedling in Melasma. Dermatologic Surgery, Publish Ahead of Print. doi: 10.1097/dss.0000000000002520 |
Microneedling + 4% TXA vs 4% HQ |
n=70, 12-week single blind randomized clinical trial showed that the two groups decreased MASI score significantly and there is no difference between two groups. Note: both groups used SPF 30 every 2 hours during the day. |
Shamsi Meymandi, S., Mozayyeni, A., Shamsi Meymandi, M., & Aflatoonian, M. (2020). Efficacy of microneedling plus topical 4% tranexamic acid solution vs 4% hydroquinone in the treatment of melasma: A single-blind randomized clinical trial. Journal Of Cosmetic Dermatology. doi: 10.1111/jocd.13392 |
3% TXA, 2% Galactomyces Ferment Filtrate, 4% Niacinamide, 2% Alpha Arbutin VS 4% Hydroquinone |
n=44, 4-week Double blind, randomized controlled clinical trial showing that TXA combination is superior to 4% hydroquinone in brightening efficacy without side effects. Notes: Level A; Good Quality Needs a bigger sample size, comparison with TCC instead of 4% HQ alone would be more useful |
Anwar, A., Wahab, S., Widita, W., Nurdin, A., Budhiani, S., & Seweng, A. (2020). Tranexamic Acid Versus Hydroquinone as a Whitening Agent | PRIME Journal. Retrieved 31 August 2020, from https://www.prime-journal.com/tranexamic-acid-versus-hydroquinone-as-a-whitening-agent/ |
Microneedling + TXA vs Microneedling + Vit C |
n=30, 4-week trial. Pigmentation decreased in both but telangiectasia only significantly improved in MN+TXA |
Amer, M. A., Mostafa, W. Z., & Tahoun, A. I. (2021). Dermoscopic evaluation of tranexamic acid versus vitamin C, with microneedling in the treatment of melasma: A comparative, split-face, single-blinded study. The Journal of Dermatological Treatment, 1–29. |
References:
-
Sadako N, Treatment of melasma with tranexamic acid, (1979) The Clin Rep ; 13: 3129- 31 ↩︎
-
Zhang, L., Tan, W., Fang, Q., Zhao, W., Zhao, Q., Gao, J., & Wang, X. (2018). Tranexamic Acid for Adults with Melasma: A Systematic Review and Meta-Analysis. Biomed Research International, 2018, 1-13. doi: 10.1155/2018/1683414 ↩︎
-
Lautenschläger H, Haut ohne Makel – Wirkstoffe und Wirksysteme, Medical Beauty Forum 2014; 5: 32-35 ↩︎
-
Cestari, T. F., Hexsel, D., Viegas, M. L., Azulay, L., Hassun, K., Almeida, A. R., Rêgo, V. R., Mendes, A. M., Filho, J. W., & Junqueira, H. (2006). Validation of a melasma quality of life questionnaire for Brazilian Portuguese language: the MelasQoL-BP study and improvement of QoL of melasma patients after triple combination therapy. The British journal of dermatology, 156 Suppl 1, 13–20. https://doi.org/10.1111/j.1365-2133.2006.07591.x ↩︎
-
Gupta, A. K., Gover, M. D., Nouri, K., Taylor, S. (2006) J. Am. Acad. Dermatol. 55(6), 1048. and M. Rendon, M. Berneburg, I. Arellano, M. Picardo, (2006) J. Am. Acad. Dermatol. 54(5 Suppl 2), S272. ↩︎
-
Ng, S., Marcant, M., & Davis, A. (2020). In vitro human skin concentrations following topical application of 2% tranexamic acid in co‐enhancer cream and branded cream formulations. Journal Of Cosmetic Dermatology. doi: 10.1111/jocd.13301 ↩︎
-
Takashima A, Yasuda S, Mizuno N. Determination of the action spectrum for UV‑induced plasminogen activator synthesis in mouse keratinocytes in vitro. J Dermatol Sci 1992;4:11‑7. ↩︎ ↩︎
-
Jensen, P., John, M., & Baird, J. (1990). Urokinase and tissue type plasminogen activators in human keratinocyte culture. Experimental Cell Research, 187(1), 162-169. doi: 10.1016/0014-4827(90)90131-s ↩︎ ↩︎
-
Rivkah Isseroff, R., & Rifkin, D. (1983). Plasminogen Is Present in the Basal Layer of the Epidermis. Journal Of Investigative Dermatology, 80(4), 297-299. doi: 10.1111/1523-1747.ep12534677 ↩︎
-
Syrovets, T., Lunov, O., & Simmet, T. (2012). Plasmin as a proinflammatory cell activator. Journal of leukocyte biology, 92(3), 509–519. https://doi.org/10.1189/jlb.0212056 ↩︎
-
Nakano, T., Fujita, H., Kikuchi, N., & Arita, H. (1994). Plasmin Converts Pro-Form of Group-I Phospholipase A2 into Receptor-Binding, Active Forms. Biochemical And Biophysical Research Communications, 198(1), 10-15. doi: 10.1006/bbrc.1994.1002 ↩︎
-
Cejkova J, Lojda Z. The damaging effect of UV rays below 320 nm on the rabbit anterior eye segment. II. Enzyme histochemical changes and plasmin activity after prolonged irradiation. Acta Histochem 1995; 97: 183–8. ↩︎
-
TOMITA, Y., MAEDA, K., & TAGAMI, H. (1992). Melanocyte-Stimulating Properties of Arachidonic Acid Metabolites: Possible Role in Postinflammatory Pigmentation. Pigment Cell Research, 5(5), 357-361. doi: 10.1111/j.1600-0749.1992.tb00562.x ↩︎
-
TOMITA, Y., MAEDA, K., & TAGAMI, H. (1988). Leukotrienes and thromboxane B2 stimulate normal human melanocytes in vitro: Possible inducers of postinflammatory pigmentation. The Tohoku Journal Of Experimental Medicine, 156(3), 303-304. doi: 10.1620/tjem.156.303. ↩︎
-
Calapai, G. (2015). Systematic Review of Tranexamic Acid Adverse Reactions. Journal Of Pharmacovigilance, 03(04). doi: 10.4172/2329-6887.1000171 ↩︎
-
Atefi, N., Dalvand, B., Ghassemi, M., Mehran, G., & Heydarian, A. (2017). Therapeutic Effects of Topical Tranexamic Acid in Comparison with Hydroquinone in Treatment of Women with Melasma. Dermatology And Therapy, 7(3), 417-424. doi: 10.1007/s13555-017-0195-0 ↩︎
-
Syrovets, T., Jendrach, M., Rohwedder, A., Schüle, A., & Simmet, T. (2001). Plasmin-induced expression of cytokines and tissue factor in human monocytes involves AP-1 and IKKbeta-mediated NF-kappaB activation. Blood, 97(12), 3941–3950. https://doi.org/10.1182/blood.v97.12.3941 ↩︎
-
Burysek, L., Syrovets, T., & Simmet, T. (2002). The serine protease plasmin triggers expression of MCP-1 and CD40 in human primary monocytes via activation of p38 MAPK and janus kinase (JAK)/STAT signaling pathways. The Journal of biological chemistry, 277(36), 33509–33517. https://doi.org/10.1074/jbc.M201941200 ↩︎
-
Matsumura, Y., Takada, K., Murakami, A., Takaoka, M., & Morimoto, S. (1996). Plasmin stimulates expression of endothelin-1 mRNA and endothelin-1 release in vascular endothelial cells. Life sciences, 58(13), 1067–1074. https://doi.org/10.1016/0024-3205(96)00060-4 ↩︎
-
Naldini, L., Tamagnone, L., Vigna, E., Sachs, M., Hartmann, G., Birchmeier, W., Daikuhara, Y., Tsubouchi, H., Blasi, F., & Comoglio, P. M. (1992). Extracellular proteolytic cleavage by urokinase is required for activation of hepatocyte growth factor/scatter factor. The EMBO journal, 11(13), 4825–4833. ↩︎
-
Hashimoto, K., Prystowsky, J., Baird, J., Lazarus, G., & Jensen, P. (1988). Keratinocyte Urokinase-Type Plasminogen Activator is Secreted as a Single Chain Precursor. Journal Of Investigative Dermatology, 90(6), 823-828. doi: 10.1111/1523-1747.ep12462057. ↩︎
-
Green, H. (1977). Terminal differentiation of cultured human epidermal cells. Cell, 11(2), 405-416. doi: 10.1016/0092-8674(77)90058-7 ↩︎
-
Morioka, S., Lazarus, G., Baird, J., & Jensen, P. (1987). Migrating Keratinocytes Express Urokinase-Type Plasminogen Activator. Journal Of Investigative Dermatology, 88(4), 418-423. doi: 10.1111/1523-1747.ep12469754 ↩︎
-
HASHIMOTO, K., HORIKOSHI, T., NISHIOKA, K., YOSHIKAWA, K., & CARTER, D. (1986). Plasminogen activator secreted by cultured human melanocytes. British Journal Of Dermatology, 115(2), 205-209. doi: 10.1111/j.1365-2133.1986.tb05719.x ↩︎
-
Maeda, K., & Tomita, Y. (2007). Mechanism of the Inhibitory Effect of Tranexamic Acid on Melanogenesis in Cultured Human Melanocytes in the Presence of Keratinocyte-conditioned Medium. JOURNAL OF HEALTH SCIENCE, 53(4), 389-396. doi: 10.1248/jhs.53.389 ↩︎ ↩︎
-
Maeda, K., & Naganuma, M. (1998). Topical trans-4-aminomethylcyclohexanecarboxylic acid prevents ultraviolet radiation-induced pigmentation. Journal Of Photochemistry And Photobiology B: Biology, 47(2-3), 136-141. doi: 10.1016/s1011-1344(98)00212-7 ↩︎
-
Peterson, R., Krull, P., Finley, P., & Ettinger, M. (1970). Changes in Antithrombin III and Plasminogen Induced by Oral Contraceptives. American Journal Of Clinical Pathology, 53(4), 468-473. doi: 10.1093/ajcp/53.4.468. ↩︎
-
Murase, D., Hachiya, A., Takano, K., Hicks, R., Visscher, M., & Kitahara, T. et al. (2013). Autophagy Has a Significant Role in Determining Skin Color by Regulating Melanosome Degradation in Keratinocytes. Journal Of Investigative Dermatology, 133(10), 2416-2424. doi: 10.1038/jid.2013.165 ↩︎
-
Alers, S., Löffler, A. S., Wesselborg, S., & Stork, B. (2012). Role of AMPK-mTOR-Ulk1/2 in the regulation of autophagy: cross talk, shortcuts, and feedbacks. Molecular and cellular biology, 32(1), 2–11. https://doi.org/10.1128/MCB.06159-11 ↩︎
-
Ye, Y., Chu, J. H., Wang, H., Xu, H., Chou, G. X., Leung, A. K., Fong, W. F., & Yu, Z. L. (2010). Involvement of p38 MAPK signaling pathway in the anti-melanogenic effect of San-bai-tang, a Chinese herbal formula, in B16 cells. Journal of ethnopharmacology, 132(2), 533–535. https://doi.org/10.1016/j.jep.2010.09.007 ↩︎
-
Kim, E. S., Shin, J. H., Seok, S. H., Kim, J. B., Chang, H., Park, S. J., Jo, Y. K., Choi, E. S., Park, J. S., Yeom, M. H., Lim, C. S., & Cho, D. H. (2013). Autophagy mediates anti-melanogenic activity of 3’-ODI in B16F1 melanoma cells. Biochemical and biophysical research communications, 442(3-4), 165–170. https://doi.org/10.1016/j.bbrc.2013.11.048 ↩︎
-
Wu, L. C., Lin, Y. Y., Yang, S. Y., Weng, Y. T., & Tsai, Y. T. (2011). Antimelanogenic effect of c-phycocyanin through modulation of tyrosinase expression by upregulation of ERK and downregulation of p38 MAPK signaling pathways. Journal of biomedical science, 18(1), 74. https://doi.org/10.1186/1423-0127-18-74 ↩︎
-
Funderburk, S. F., Wang, Q. J., & Yue, Z. (2010). The Beclin 1-VPS34 complex–at the crossroads of autophagy and beyond. Trends in cell biology, 20(6), 355–362. https://doi.org/10.1016/j.tcb.2010.03.002 ↩︎
-
Obara, K., & Ohsumi, Y. (2008). Dynamics and function of PtdIns(3)P in autophagy. Autophagy, 4(7), 952–954. https://doi.org/10.4161/auto.6790 ↩︎
-
Miracco, C., Cevenini, G., Franchi, A., Luzi, P., Cosci, E., & Mourmouras, V. et al. (2010). Beclin 1 and LC3 autophagic gene expression in cutaneous melanocytic lesions. Human Pathology, 41(4), 503-512. doi: 10.1016/j.humpath.2009.09.004 ↩︎
-
Raposo, G., & Marks, M. (2007). Melanosomes — dark organelles enlighten endosomal membrane transport. Nature Reviews Molecular Cell Biology, 8(10), 786-797. doi: 10.1038/nrm2258 and Ho, H., & Ganesan, A. (2011). The pleiotropic roles of autophagy regulators in melanogenesis. Pigment Cell & Melanoma Research, 24(4), 595-604. doi: 10.1111/j.1755-148x.2011.00889.x ↩︎
-
Cho, Y., Park, J., Lim, D., & Lee, J. (2017). Tranexamic acid inhibits melanogenesis by activating the autophagy system in cultured melanoma cells. Journal Of Dermatological Science, 88(1), 96-102. doi: 10.1016/j.jdermsci.2017.05.019 ↩︎
-
Zhang, X., Yang, X., Yang, H., & Yang, Y. (2003). Study of inhibitory effect of acidum tranexamicum on melanin synthesis. Chin J Dermatovenereol Integr Tradit West Med., 2, 227-9. ↩︎
-
Seo, S., Cho, S., Cho, W., Jung, M., Ro, S., Kim, M., & Hong, C. (2007). Effect of Trans-4-Aminomethylcyclohexanecarboxylic Acid on the Proliferation and Melanization in Cultured Normal Human Melanocytes. Annals Of Dermatology, 19(2), 60. doi: 10.5021/ad.2007.19.2.60 ↩︎
-
Ferrara N. (2010) Binding to the extracellular matrix and proteolytic processing: two key mechanisms regulating vascular endothelial growth factor action. Mol Biol Cell; 21: 687–690 ↩︎
-
Falcone, D. J., McCaffrey, T. A., Haimovitz-Friedman, A., Vergilio, J. A., & Nicholson, A. C. (1993). Macrophage and foam cell release of matrix-bound growth factors. Role of plasminogen activation. The Journal of biological chemistry, 268(16), 11951–11958. ↩︎
-
Passeron T. (2013) Melasma pathogenesis and influencing factors – An overview of the latest research. J Eur Acad Dermatol Venereol, 27 Suppl 1:5‑6. ↩︎
-
Kim EH, Kim YC, Lee ES, Kang HY. (2007) The vascular characteristics of melasma. J Dermatol Sci, 46:111‑6. ↩︎ ↩︎
-
Sonthalia S. (2015) Etiopathogenesis of melasma. In: Sarkar R, editor. Melasma: A Monograph. New Delhi: Jaypee, p. 6‑14. ↩︎
-
Kal, H. B., Struikmans, H., Gebbink, M. F., & Voest, E. E. (2004). Response of rat prostate and lung tumors to ionizing radiation combined with the angiogenesis inhibitor AMCA. Strahlentherapie und Onkologie : Organ der Deutschen Rontgengesellschaft … [et al], 180(12), 798–804. https://doi.org/10.1007/s00066-004-1276-4 ↩︎
-
Bastaki, M., Nelli, E. E., Dell’Era, P., Rusnati, M., Molinari-Tosatti, M. P., Parolini, S., Auerbach, R., Ruco, L. P., Possati, L., & Presta, M. (1997). Basic fibroblast growth factor-induced angiogenic phenotype in mouse endothelium. A study of aortic and microvascular endothelial cell lines. Arteriosclerosis, thrombosis, and vascular biology, 17(3), 454–464. https://doi.org/10.1161/01.atv.17.3.454 ↩︎
-
Imokawa, G., Miyagishi, M., & Yada, Y. (1995). Endothelin-1 as a new melanogen: coordinated expression of its gene and the tyrosinase gene in UVB-exposed human epidermis. The Journal of investigative dermatology, 105(1), 32–37. https://doi.org/10.1111/1523-1747.ep12312500 ↩︎
-
Imokawa, G., Kobayashi, T., Miyagishi, M., Higashi, K., & Yada, Y. (1997). The role of endothelin-1 in epidermal hyperpigmentation and signaling mechanisms of mitogenesis and melanogenesis. Pigment cell research, 10(4), 218–228. https://doi.org/10.1111/j.1600-0749.1997.tb00488.x ↩︎
-
Iddamalgoda, A., Le, Q. T., Ito, K., Tanaka, K., Kojima, H., & Kido, H. (2008). Mast cell tryptase and photoaging: possible involvement in the degradation of extra cellular matrix and basement membrane proteins. Archives of dermatological research, 300 Suppl 1, S69–S76. https://doi.org/10.1007/s00403-007-0806-1 ↩︎
-
Crivellato, E., Nico, B., & Ribatti, D. (2008). Mast cells and tumour angiogenesis: new insight from experimental carcinogenesis. Cancer letters, 269(1), 1–6. https://doi.org/10.1016/j.canlet.2008.03.031 ↩︎
-
Grimbaldeston, M. A., Simpson, A., Finlay-Jones, J. J., & Hart, P. H. (2003). The effect of ultraviolet radiation exposure on the prevalence of mast cells in human skin. The British journal of dermatology, 148(2), 300–306. https://doi.org/10.1046/j.1365-2133.2003.05113.x ↩︎
-
Gonzalez, S., Moran, M., & Kochevar, I. E. (1999). Chronic photodamage in skin of mast cell-deficient mice. Photochemistry and photobiology, 70(2), 248–253. ↩︎
-
Na, J., Choi, S., Yang, S., Choi, H., Kang, H., & Park, K. (2012). Effect of tranexamic acid on melasma: a clinical trial with histological evaluation. Journal Of The European Academy Of Dermatology And Venereology, 27(8), 1035-1039. doi: 10.1111/j.1468-3083.2012.04464.x ↩︎
-
Sano, T., Kume, T., Fujimura, T., Kawada, H., Higuchi, K., Iwamura, M., Hotta, M., Kitahara, T., & Takema, Y. (2009). Long-term alteration in the expression of keratins 6 and 16 in the epidermis of mice after chronic UVB exposure. Archives of dermatological research, 301(3), 227–237. https://doi.org/10.1007/s00403-008-0914-6 ↩︎
-
Denda, M., Kitamura, K., Elias, P. M., & Feingold, K. R. (1997). trans-4-(Aminomethyl)cyclohexane carboxylic acid (T-AMCHA), an anti-fibrinolytic agent, accelerates barrier recovery and prevents the epidermal hyperplasia induced by epidermal injury in hairless mice and humans. The Journal of investigative dermatology, 109(1), 84–90. https://doi.org/10.1111/1523-1747.ep12276640 ↩︎
-
Morita, K., Miyachi, Y., & Furuse, M. (2011). Tight junctions in epidermis: from barrier to keratinization. European journal of dermatology : EJD, 21(1), 12–17. https://doi.org/10.1684/ejd.2010.1192 ↩︎
-
Yuki, T., Hachiya, A., Kusaka, A., Sriwiriyanont, P., Visscher, M. O., Morita, K., Muto, M., Miyachi, Y., Sugiyama, Y., & Inoue, S. (2011). Characterization of tight junctions and their disruption by UVB in human epidermis and cultured keratinocytes. The Journal of investigative dermatology, 131(3), 744–752. https://doi.org/10.1038/jid.2010.385 ↩︎
-
Yamamoto, T., Kurasawa, M., Hattori, T., Maeda, T., Nakano, H., & Sasaki, H. (2008). Relationship between expression of tight junction-related molecules and perturbed epidermal barrier function in UVB-irradiated hairless mice. Archives of dermatological research, 300(2), 61–68. https://doi.org/10.1007/s00403-007-0817-y ↩︎
-
Katsuta, Y., Yoshida, Y., Kawai, E., Suetsugu, M., Kohno, Y., Inomata, S., & Kitamura, K. (2005). trans-4-(Aminomethyl)cyclohexane carboxylic acid methylamide (t-AMCHA methylamide) inhibits the physical interaction between urokinase-type plasminogen activator and stratum corneum, and accelerates the recovery of barrier function. Journal of dermatological science, 40(3), 218–220. https://doi.org/10.1016/j.jdermsci.2005.10.004 ↩︎
-
Yuan, C., Wang, X., Yang, L., & Wu, P. (2013). Tranexamic acid accelerates skin barrier recovery and upregulates occludin in damaged skin. International Journal Of Dermatology, 53(8), 959-965. doi: 10.1111/ijd.12099 ↩︎ ↩︎
-
Demerjian, M., Hachem, J., Tschachler, E., Denecker, G., Declercq, W., & Vandenabeele, P. et al. (2008). Acute Modulations in Permeability Barrier Function Regulate Epidermal Cornification. The American Journal Of Pathology, 172(1), 86-97. doi: 10.2353/ajpath.2008.070161 ↩︎
-
Stefansson, K., Brattsand, M., Roosterman, D., Kempkes, C., Bocheva, G., Steinhoff, M., & Egelrud, T. (2008). Activation of Proteinase-Activated Receptor-2 by Human Kallikrein-Related Peptidases. Journal Of Investigative Dermatology, 128(1), 18-25. doi: 10.1038/sj.jid.5700965 ↩︎
-
Hachem, J., Houben, E., Crumrine, D., Man, M., Schurer, N., & Roelandt, T. et al. (2006). Serine Protease Signaling of Epidermal Permeability Barrier Homeostasis. Journal Of Investigative Dermatology, 126(9), 2074-2086. doi: 10.1038/sj.jid.5700351 ↩︎
-
Yamasaki, K., Di Nardo, A., Bardan, A., Murakami, M., Ohtake, T., & Coda, A. et al. (2007). Increased serine protease activity and cathelicidin promotes skin inflammation in rosacea. Nature Medicine, 13(8), 975-980. doi: 10.1038/nm1616 ↩︎
-
Meyer-Hoffert, U., & Schröder, J. (2011). Epidermal Proteases in the Pathogenesis of Rosacea. Journal Of Investigative Dermatology Symposium Proceedings, 15(1), 16-23. doi: 10.1038/jidsymp.2011.2 ↩︎
-
Steinhoff, M., Buddenkotte, J., Aubert, J., Sulk, M., Novak, P., & Schwab, V. et al. (2011). Clinical, Cellular, and Molecular Aspects in the Pathophysiology of Rosacea. Journal Of Investigative Dermatology Symposium Proceedings, 15(1), 2-11. doi: 10.1038/jidsymp.2011.7 ↩︎
-
Lee, S., Jeong, S., & Lee, S. (2010). Protease and Protease-Activated Receptor-2 Signaling in the Pathogenesis of Atopic Dermatitis. Yonsei Medical Journal, 51(6), 808. doi: 10.3349/ymj.2010.51.6.808 ↩︎
-
Winter, M., Shasby, S., Ries, D., & Shasby, D. (2006). PAR2 activation interrupts E-cadherin adhesion and compromises the airway epithelial barrier: protective effect of β-agonists. American Journal Of Physiology-Lung Cellular And Molecular Physiology, 291(4), L628-L635. doi: 10.1152/ajplung.00046.2006 ↩︎
-
Tunggal, J., Helfrich, I., Schmitz, A., Schwarz, H., Günzel, D., & Fromm, M. et al. (2005). E-cadherin is essential for in vivo epidermal barrier function by regulating tight junctions. The EMBO Journal, 24(6), 1146-1156. doi: 10.1038/sj.emboj.7600605 ↩︎
-
Tinkle, C., Pasolli, H., Stokes, N., & Fuchs, E. (2008). New insights into cadherin function in epidermal sheet formation and maintenance of tissue integrity. Proceedings Of The National Academy Of Sciences, 105(40), 15405-15410. doi: 10.1073/pnas.0807374105 ↩︎
-
Zhong, S., Sun, N., Liu, H., Niu, Y., Chen, C., & Wu, Y. (2015). Topical tranexamic acid improves the permeability barrier in rosacea. Dermatologica Sinica, 33(2), 112-117. doi: 10.1016/j.dsi.2015.04.012 ↩︎
-
Bageorgou, F., Vasalou, V., Tzanetakou, V., & Kontochristopoulos, G. (2019). The new therapeutic choice of tranexamic acid solution in treatment of erythematotelangiectatic rosacea. Journal of cosmetic dermatology, 18(2), 563–567. https://doi.org/10.1111/jocd.12724 ↩︎
